
08 Apr What You Need To Know About Heel Pain
Heel pain is most common to occur in those aged 30 years and older. Often the first steps out of bed in the morning are the worst, or after sitting for a period of time but also, pain may worsen when standing and walking.
The start of heel pain often follows a change in loading on the body – this may be a sudden increase in walking (e.g. walking while sightseeing on holidays), an increase in body-weight, an increase in exercise (e.g. going for a run when you haven’t run in a couple of months) or a change in shoes (e.g. wearing flexible Nike Free Runs after wearing Asics Keyano for the past year).
Some other factors which also have a large impact on heel pain include:
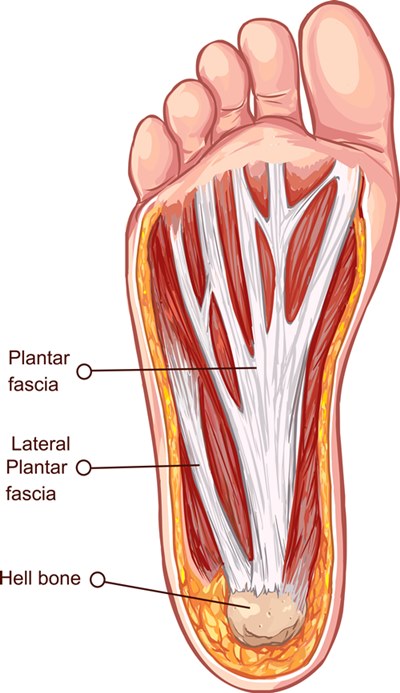
- Tight calf muscles – The calf muscles attach to the heel bone via the Achilles tendon, where fibres have been found to directly connect to the plantar fascia on the bottom of the feet. The plantar fascia is a ligament-like structure on the bottom of the feet which originates at the heel bone, runs along the foot and inserts into the toes – it tightens during gait (walking) to help with propulsion. If the calf muscles are tight there is a “pulling” at the insertion of the plantar fascia at the heel bone, creating inflammation and pain, which over time leads to degeneration of the plantar fascia – most people know this as plantar fasciitis.
- Hypermobility – The ligaments which connects bone to bone. Some people have ligaments more like elastic bands and others like steel cables – this is a genetic factor due to the collagen in the ligaments. Hypermobile patients typically have a flatter foot, which ‘over-pronates (rolls in excessively) more than someone who is less hypermobile. As a result, hypermobile patients typically will have tighter muscles and are more prone to soft tissue injuries (e.g. always rolling ankles, bunions, etc.). In heel pain, often this ‘over-pronation’ leads to a stretching of the plantar fascia, causing degeneration and pain and added to this, the hypermobile patient will have tight calf muscles which further exacerbates the condition.
- Foot type – No foot type is spared from heel pain, you might have a high-arch, neutral or flat foot type. From clinical experience, we do often see patients with a flatter foot type that will develop heel pain.
What can you do?
Research has shown us that most cases of heel pain (more specifically plantar fasciitis) will self-resolve within 12 months – but that is a long time to be in pain and not everyone will be that lucky! Interestingly, studies have shown that the natural course of heel pain is to improve, worsen, improve, worsen and so on. This causes a frenzy on the internet because there are a lot of suggestions out there where people claim to have fixed their plantar fasciitis (e.g. some people claim covering their feet in cabbage or soaking their feet in vinegar helped cure their plantar fasciitis). What is happening in these cases is that the person tries something new and their pain worsens over time, so they blame that modality for making their pain worse and try something new, such as applying cabbage to their feet, then the pain improves – due to the natural progression of the condition and they attribute the cabbage to curing their pain! This is why randomised control studies are so important – because they measure an intervention against a control group (i.e. group with no intervention) and then calculate if the intervention actually does have a clinically significant impact vs the control group.
Treatment
What you can do at home:
- Rest or activity modification (e.g. swim instead of run)
- Ice
- Anti-inflammatories
- Gel heel cups – purchased from your local pharmacy
- Stretching – stretch calf muscles at least twice per day
- Footwear modification – firmer shoes with more support and cushioning under the heel
What our Podiatrists will do:
- Unload structures – taping, stretching regiment, footwear and orthotics or immobilisation boot
- Increase load on tissues – high load strength training for plantarfasciopathy
- Facilitate healing – extracorporeal shockwave therapy, dry needling, massage
If you want some expert advise about your podiatry problems or just want to get back on track straight away, contact Sydney Sports Podiatry or book an appointment now.
Thanks for reading,
Sydney Sports Podiatry
1300 474 306



